Contact Dermatitis
Background
Contact dermatitis is a common work-related disease. It is an itchy or painful inflammatory skin reaction that looks like a rash or burn. It can present in mild forms, such as dryness with reddening, chapping and scaling, as well as in more severe forms, such as eczema-like dermatitis with swelling, blisters or fissures. It typically affects the hands, making it painful to continue work.
The Centre for Research Expertise in Occupational Disease (CREOD) reports that only 62% of contact dermatitis patients at their occupational disease clinic in Toronto returned to work 6 months after skin assessment. Of those who had returned to work, about one-third had changed jobs due to their skin problem.
Occupational risk factors
-
- Wet work* [2]
- Certain cleaning agents (soaps, shampoo, detergents) [2]
- Organic solvents [2]
- Chronic mechanical and frictional stress [2]
- Metalworking fluids [2]
- Rubber additives [2]
- Acids and alkalis [2]
- Isothiazolinone [3]
*Wet work is the main risk factor for occupational contact dermatitis. It involves extensive hand washing (more than 20 times per shift), immersing the hands in water for more than 2 hours per shift, or wearing gloves for extended periods. Prolonged exposure to wet work disrupts the natural barrier in the skin, allowing sensitizing agents to pass through the skin more easily and cause skin allergies.
Key Findings
The greatest risk of contact dermatitis was observed among barbers and hairdressers, and workers in metal machining occupations.
Barbers and hairdressers
 Hairdressers are particularly vulnerable to developing dermatitis because they are regularly exposed to both wet work and chemicals (e.g., soaps, shampoos, hair dye, cleaning agents).
Hairdressers are particularly vulnerable to developing dermatitis because they are regularly exposed to both wet work and chemicals (e.g., soaps, shampoos, hair dye, cleaning agents).
-
- Barbers and hairdressers: 1.48 times the risk
Nurses
 Nursing and relating occupations in the ODSS had consistently decreased risks of dermatitis despite being recognized as a high-risk group with a high prevalence of dermatitis. This may be explained by the prevention measures put in place to reduce exposure to, and effects of, natural rubber latex in Western industrialized countries. Prevention measures, such as use of gloves or skin barrier creams in wet activities and hand alcohol instead of soap and water as disinfectant have been promoted in healthcare [4,5]. Additionally, healthcare workers may not seek treatment for dermatitis, opting instead to self-manage until their skin condition resolves and are therefore not captured in health outcome data in the ODSS [6]. Only workers in ‘Other occupations in medicine and health, nec’ had an increased risk of dermatitis in the ODSS.
Nursing and relating occupations in the ODSS had consistently decreased risks of dermatitis despite being recognized as a high-risk group with a high prevalence of dermatitis. This may be explained by the prevention measures put in place to reduce exposure to, and effects of, natural rubber latex in Western industrialized countries. Prevention measures, such as use of gloves or skin barrier creams in wet activities and hand alcohol instead of soap and water as disinfectant have been promoted in healthcare [4,5]. Additionally, healthcare workers may not seek treatment for dermatitis, opting instead to self-manage until their skin condition resolves and are therefore not captured in health outcome data in the ODSS [6]. Only workers in ‘Other occupations in medicine and health, nec’ had an increased risk of dermatitis in the ODSS.
-
- Other occupations in medicine and health, not elsewhere classified*: 1.36 times the risk
- Nurses, registered, graduate and nurses-in-training: 0.82 times the risk
- Nursing assistants: 0.73 times the risk
- Nursing aides and orderlies: 0.99 times the risk
- Nursing, therapy and related assisting occupations, not elsewhere classified: 0.90 times the risk
*This group includes occupations, not elsewhere classified, concerned with activities in medicine and health, such as: designing, making, assembling and fitting prosthetic devices; operating inhalation therapy, electroencephalographic, orthoptic, electrocardiographic and other hospital, equipment; controlling infection and assisting professional staff in clinics, pharmacies, morgues and animal hospitals; sterilizing and packaging hospital supplies and assisting in preparation of special diet menus.
Food and beverage workers
 Food-handlers are required to wash their hands frequently and may wear gloves to prevent the spread of foodborne illness. They also clean food preparation equipment and surfaces using various cleaning agents and detergents that could increase their risk of contact dermatitis. Workers in food and beverage industries and laboring occupations may also be at increased risk of contact dermatitis due to exposure to chronic mechanical and frictional stress combined with wet work exposure.
Food-handlers are required to wash their hands frequently and may wear gloves to prevent the spread of foodborne illness. They also clean food preparation equipment and surfaces using various cleaning agents and detergents that could increase their risk of contact dermatitis. Workers in food and beverage industries and laboring occupations may also be at increased risk of contact dermatitis due to exposure to chronic mechanical and frictional stress combined with wet work exposure.
-
- Occupations in labouring and other elemental work: food, beverage and related processing: 1.20 times the risk
- Food, beverage and related processing occupations, not elsewhere classified: 1.15 times the risk
- Food and beverage preparation and related services: 1.05 times the risk
- Food and beverage industries: 1.11 times the risk
Painters
Painters can be exposed to a variety of paints and coatings which may be risk factors for contact dermatitis. Isothiazolinones, which are used as biocides in paints, can cause allergic contact dermatitis [3].
-
- Painting and decorating occupations, except construction: 1.29 times the risk
Metal machining and metal products fabricating and assembling occupations
 Chronic mechanical and frictional stress and exposure to solvents, oils, metal working fluids, and chlorinated agents are important exposures for contact dermatitis for metal machining and product fabricating occupations [7,8].
Chronic mechanical and frictional stress and exposure to solvents, oils, metal working fluids, and chlorinated agents are important exposures for contact dermatitis for metal machining and product fabricating occupations [7,8].
-
- Metal machining occupations: 1.27 times the risk
- Foremen/forewomen, metal machining occupations: 1.89 times the risk
- Machinist and machine-tool setting-up occupations: 1.30 times the risk
- Metal shaping and forming occupations, except machining: 1.07 times the risk
- Metalworking-machine operators, not elsewhere classified: 1.14 times the risk
- Metal products fabricating and assembling occupations, not elsewhere classified: 1.15 times the risk
- Motor vehicle fabricating and assembling occupations, not elsewhere classified: 1.22 times the risk
- Metal machining occupations: 1.27 times the risk
Relative Risk by Industry and Occupation
Figure 1. Risk of dermatitis diagnosis among workers employed in each industry group relative to all others, Occupational Disease Surveillance System (ODSS), 1999-2016
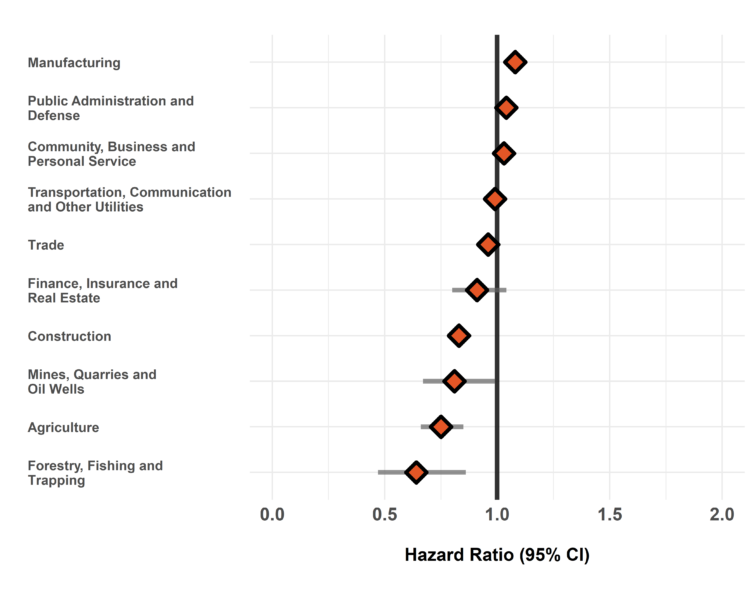
The hazard ratio is an estimate of the average time to diagnosis among workers in each industry/occupation group divided by that in all others during the study period. Hazard ratios above 1.00 indicate a greater risk of disease in a given group compared to all others. Estimates are adjusted for birth year and sex. The width of the 95% Confidence Interval (CI) is based on the number of cases in each group (more cases narrows the interval).
Figure 2. Risk of dermatitis diagnosis among workers employed in each occupation group relative to all others, Occupational Disease Surveillance System (ODSS), 1999-2016
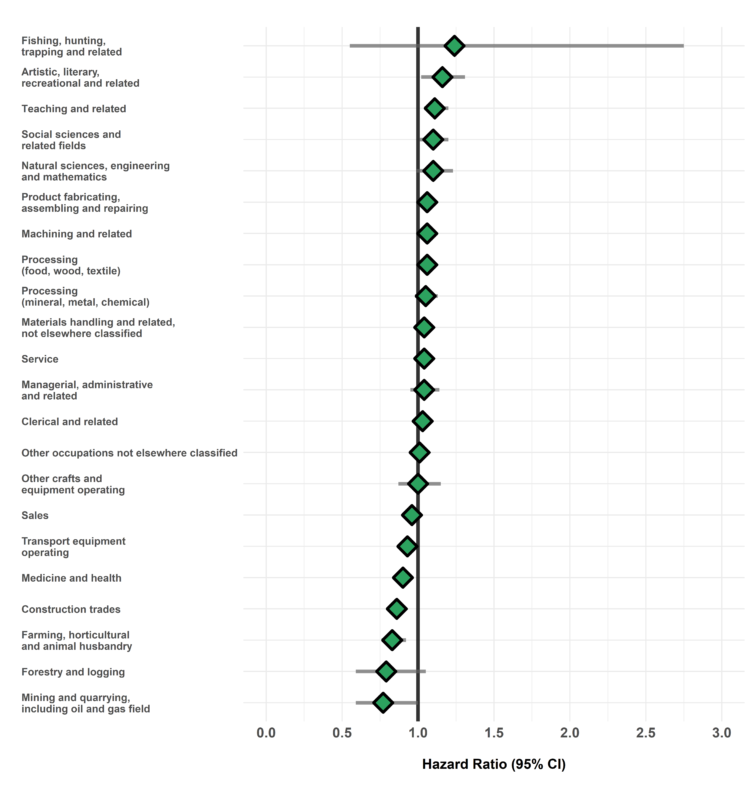
The hazard ratio is an estimate of the average time to diagnosis among workers in each industry/occupation group divided by that in all others during the study period. Hazard ratios above 1.00 indicate a greater risk of disease in a given group compared to all others. Estimates are adjusted for birth year and sex. The width of the 95% Confidence Interval (CI) is based on the number of cases in each group (more cases narrows the interval).
Table of Results
Table 1. Surveillance of Dermatitis: Number of cases, workers employed, and hazard ratios in each industry (SIC)
| SIC Code * | Industry Group | Number of cases | Number of workers employed | Hazard Ratio (95% CI) † |
| 1 | Agriculture | 252 | 10,055 | 0.75 (0.66-0.85) |
| 2/3 | Forestry, Fishing and Trapping |
43 | 2,125 | 0.64 (0.47-0.86) |
| 4 | Mines, Quarries and Oil Wells |
101 | 4,037 | 0.81 (0.67-0.99) |
| 5 | Manufacturing | 5,282 | 146,924 | 1.08 (1.04-1.11) |
| 6 | Construction | 1,589 | 61,003 | 0.83 (0.79-0.87) |
| 7 | Transportation, Communication and Other Utilities |
1,911 | 58,775 | 0.99 (0.94-1.04) |
| 8 | Trade | 4,374 | 129,880 | 0.96 (0.93-0.99)* |
| 9 | Finance, Insurance and Real Estate |
212 | 6,584 | 0.91 (0.80-1.04) |
| 10 | Community, Business and Personal Service |
7,203 | 187,038 | 1.03 (1.00-1.06) |
| 11 | Public Administration and Defense |
1,973 | 53,619 | 1.04 (0.99-1.09) |
| * SIC: Standard Industrial Classification (1970) | ||||
| † Hazard rate in each group relative to all others | ||||
Table 2. Surveillance of Dermatitis: Number of cases, workers employed, and hazard ratios in each occupation (CCDO) group
| CCDO Code * | Occupation Group | Number of cases | Number of workers employed | Hazard Ratio (95% CI) † |
| 11 | Managerial, administrative and related |
501 | 12,953 | 1.04 (0.95-1.14) |
| 21 | Natural sciences, engineering and mathematics |
319 | 8,742 | 1.10 (0.99-1.23) |
| 23 | Social sciences and related fields |
506 | 11,409 | 1.10 (1.01-1.20) |
| 25 | Religion | |||
| 27 | Teaching and related | 777 | 17,376 | 1.11 (1.04-1.20) |
| 31 | Medicine and health | 1,664 | 43,492 | 0.90 (0.85-0.95) |
| 33 | Artistic, literary, recreational and related |
246 | 5,966 | 1.16 (1.02-1.31) |
| 41 | Clerical and related | 2,180 | 56,458 | 1.03 (0.99-1.08) |
| 51 | Sales | 1,927 | 54,051 | 0.96 (0.91-1.00) |
| 61 | Service | 4,077 | 106,970 | 1.04 (1.01-1.08) |
| 71 | Farming, horticultural and animal husbandry |
424 | 15,454 | 0.83 (0.76-0.92) |
| 73 | Fishing, hunting, trapping and related |
6 | 156 | 1.24 (0.55-2.75) |
| 75 | Forestry and logging | 47 | 1,869 | 0.79 (0.59-1.05) |
| 77 | Mining and quarrying, including oil and gas field |
55 | 2,344 | 0.77 (0.59-1.00) |
| 81 | Processing (mineral, metal, chemical) |
754 | 21,037 | 1.05 (0.98-1.13) |
| 82 | Processing (food, wood, textile) |
1,026 | 27,287 | 1.06 (0.99-1.12) |
| 83 | Machining and related | 1,568 | 45,586 | 1.06 (1.01-1.12) |
| 85 | Product fabricating, assembling and repairing |
2,673 | 76,210 | 1.06 (1.02-1.11) |
| 87 | Construction trades | 1,577 | 59,331 | 0.86 (0.81-0.90) |
| 91 | Transport equipment operating |
1,533 | 51,591 | 0.93 (0.88-0.98) |
| 93 | Materials handling and related, not elsewhere classified |
1,355 | 39,663 | 1.04 (0.98-1.10) |
| 95 | Other crafts and equipment operating |
198 | 5,858 | 1.00 (0.87-1.15) |
| 99 | Other occupations not elsewhere classified | 1,957 | 58,101 | 1.01 (0.96-1.06) |
| * CCDO: Canadian Classification Dictionary of Occupations (1971) | ||||
| † Hazard rate in each group relative to all others | ||||
Please note that ODSS results shown here may differ from those previously published or presented. This may occur due to changes in case definitions, methodological approaches, and the ongoing nature of the surveillance cohort.
References
- Holness DL. Workers with Occupational Contact Dermatitis: Work Outcomes and Return to Work Process in the First Six Months following Diagnosis. J Allergy. 2011;2011:1–4.
- Holness DL. Occupational skin allergies: Testing and treatment (the case of occupational allergic contact dermatitis). Curr Allergy Asthma Rep. 2014;14(2).
- Herman A, Aerts O, de Montjoye L, Tromme I, Goossens A, Baeck M. Isothiazolinone derivatives and allergic contact dermatitis: a review and update. J Eur Acad Dermatol Venereol. 2019;33(2):267–76.
- Soltanipoor M, Kezic S, Sluiter JK, Rustemeyer T. The effectiveness of a skin care program for the prevention of contact dermatitis in health care workers (the Healthy Hands Project): Study protocol for a cluster randomized controlled trial. Trials. 2017;18(1):92.
- Kampf G, Löffler H. Prevention of irritant contact dermatitis among health care workers by using evidence-based hand hygiene practices: A review. Ind Health. 2007;45(5):645–52.
- Nurmohamed S, Bodley T, Thompson A, Holness DL. Health care utilization characteristics in patch test patients. Dermatitis. 2014;25(5):268–72.
- Behroozy A, Keegel TG. Wet-work exposure: A main risk factor for occupational hand dermatitis. Saf Health Work. 2014;5(4):175–80.
- Semple S, Graham M, Cowie H, Cherrie JW. The causative factors of dermatitis among workers exposed to metalworking fluids. UK Health and Safety Executive, 2007.
